Billing codes and guidelines are dynamic and should be tracked every year. For Medicare claims, the Centers for Medicare and Medicaid Services (CMS) and the Durable Medical Equipment Medicare Administrative Contractors (DME MACs) are the only authoritative sources for HCPCS Level II Coding Guidelines. CMS could potentially reassign, create, terminate or modify HCPCS codes during the stages of Product development.
Recently, (CMS) published the continuation of prior authorization (PA) for 45 Healthcare Common Procedure Coding System (HCPCS) codes on the Required Prior Authorization List of DMEPOS Items that require prior authorization as a condition of payment (Federal Register / Vol. 85, No. 28, 7666-7668).
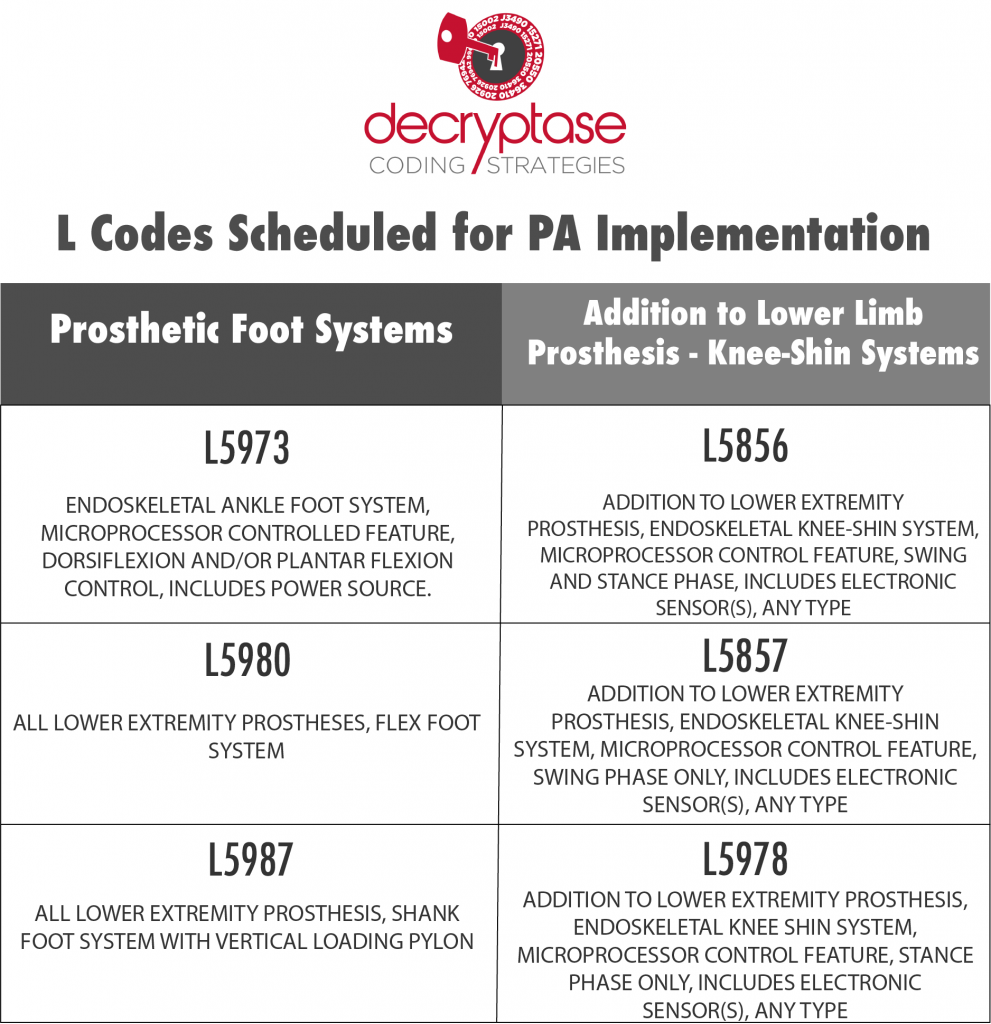
Within the list of 45 L-codes, three prosthetic foot system codes and three lower limb extremity-knee-shin prosthesis system codes are scheduled for implementation. To assist manufacturers and suppliers with correct coding, the Durable Medical Equipment Medicare Administrative Contractors (DME MACs) are issuing Coding Guidelines for these six L-codes included in the Prior Authorization Condition of Payment program:
Effective for claims with dates of service on or after 01/01/2021, the only products which may be billed using codes L5856, L5857, L5858, L5973, L5980, and L5987 are those for which a written Coding Verification Review has been made by the Pricing, Data Analysis and Coding (PDAC) Contractor and subsequently published on the appropriate Product Classification List. Correct HCPCS coding is a determination that the item provided to a beneficiary is billed using the appropriate HCPCS code for that item. Suppliers are required to correctly code for the item billed. An item/service is correctly coded when it meets all the coding guidelines listed in CMS HCPCS guidelines, LCDs, LCD-related Policy Articles, or DME MAC articles.
We can assist with the PA and benefit verifications (BVs) for your Product’s billing code to avoid denials or delays in payments. We also have the expertise to get your new product accurately coded and we have the industry relationships necessary to be effective advocates for you in your quest for coverage. Most importantly, we have a passion for what we do and the drive to see your project through.
If you need assistance with conducting a coding verification with PDAC, GIRS has over 17 years of experience submitting competent and successful coding verifications for a range of supplies and devices. Visit us at girsinc.com. We are currently offering a free Reimbursement Needs Review to address Market access and uptake during the pandemic.
Please connect with us in LinkedIn and follow our company page.
The CMS Guidance for Prosthetic Feet and Additions to Lower Limb Extremity Prostheses can be found at www.dmepdac.com
About GIRS
For more than 17 years, GIRS has been assisting medical technology manufacturers with their market uptake and reimbursement strategies so that patients can have access to the care that they need. To implement successful market access strategies, the GIRS Value Discovery Landscape Assessments® team and the Payer Advocacy Compass® team work together to develop and implement foundation reimbursement landscape and payer advocacy strategies to obtain positive coverage, appropriate payment, and innovative payer contracting arrangements to improve market uptake. For more information, email us at info@girsinc.com or call us at 901-834-9119.

